Feb 6, 2026

Uneven skin tone, dark patches, or light spots can be frustrating, especially when they appear suddenly or don’t fade over time. For many people, these changes in skin colour raise questions and concerns about their causes and treatment.
Skin pigmentation refers to the natural colouring of your skin, which is mainly determined by a substance called melanin. When melanin production or distribution is disrupted, it can lead to pigmentation disorders.
These conditions can range from mild and temporary to more noticeable and long-lasting, but the good news is that many of them are treatable.
What Is Skin Pigmentation?
Skin pigmentation is the natural colour of your skin, determined by a pigment called melanin. Melanin is produced by cells known as melanocytes, which are found in the outer layer of the skin. It not only gives your skin its colour but also helps protect it from sun damage.
When melanin is produced in too much or too little amount, or when it’s unevenly distributed, it can lead to visible changes in skin tone. These changes are known as pigmentation disorders, and they can appear as dark spots, lighter patches, or general unevenness in skin colour.

What Are the Skin Pigmentation Causes
Skin pigmentation changes can happen when the production or distribution of melanin becomes disrupted. This disruption can be caused by internal factors, such as hormones or genetics, or by external influences, such as sun exposure or skin injuries. Some causes are temporary, while others may lead to long-term changes in skin tone.
Understanding the exact cause is important because it helps determine the most suitable treatment and whether the condition is likely to recur.
Internal Causes
These causes originate from within the body and often involve hormonal or genetic factors. They may not always be preventable, but they can often be managed with proper care.
Hormonal changes
Shifts in hormone levels, especially oestrogen and progesterone, can trigger excess melanin production. A common example is melasma, which often appears during pregnancy (sometimes called the “mask of pregnancy”) or while taking hormonal contraceptives.
Genetic conditions
Some individuals inherit conditions that affect how melanin is made or distributed. For instance, albinism is a rare genetic condition in which the body produces little or no melanin, resulting in very light skin, hair, and eyes.
Autoimmune diseases
Conditions like vitiligo occur when the immune system mistakenly attacks melanocytes, causing white patches to develop on the skin. This is a chronic but non-contagious condition.
Endocrine disorders
Diseases such as Addison’s disease can increase melanin production, leading to general darkening of the skin, especially in areas like scars, folds, or joints.
Ageing
Over time, melanin can accumulate in certain areas due to long-term sun exposure, leading to age spots (also called liver spots or solar lentigines), which are more common in older adults.
External and Environmental Causes
These causes are linked to lifestyle factors, sun exposure, and external stressors that affect the skin’s surface or trigger an inflammatory response.
Sun exposure
The sun’s UV rays are the most common external trigger for pigmentation problems. They stimulate melanocytes to produce more melanin as a defence mechanism. This can lead to freckles, sunspots, or darkening of existing patches, especially in conditions such as melasma.
Post-inflammatory pigmentation
Any skin injury or inflammation, such as acne, eczema, cuts, or burns, can lead to post-inflammatory hyperpigmentation (PIH). After the skin heals, dark marks may remain for weeks or months, especially in darker skin tones.
Medications and medical treatments
Certain medications, including chemotherapy drugs, anti-malarials, and some antibiotics, can affect pigmentation. Long-term use of topical steroids may also cause lighter or darker patches to appear.
Chemical exposure or product irritation
Harsh skincare ingredients, such as alcohol-based products or those containing mercury or hydroquinone (in unsafe amounts), can irritate the skin and contribute to pigmentation disorders, especially if used without professional guidance.
Friction and repeated trauma
Repeated rubbing or pressure on the skin from tight clothing, shaving, or certain skin habits can cause thickened, darkened areas, often on the elbows, knees, or underarms.
Types of Skin Pigmentation Disorders
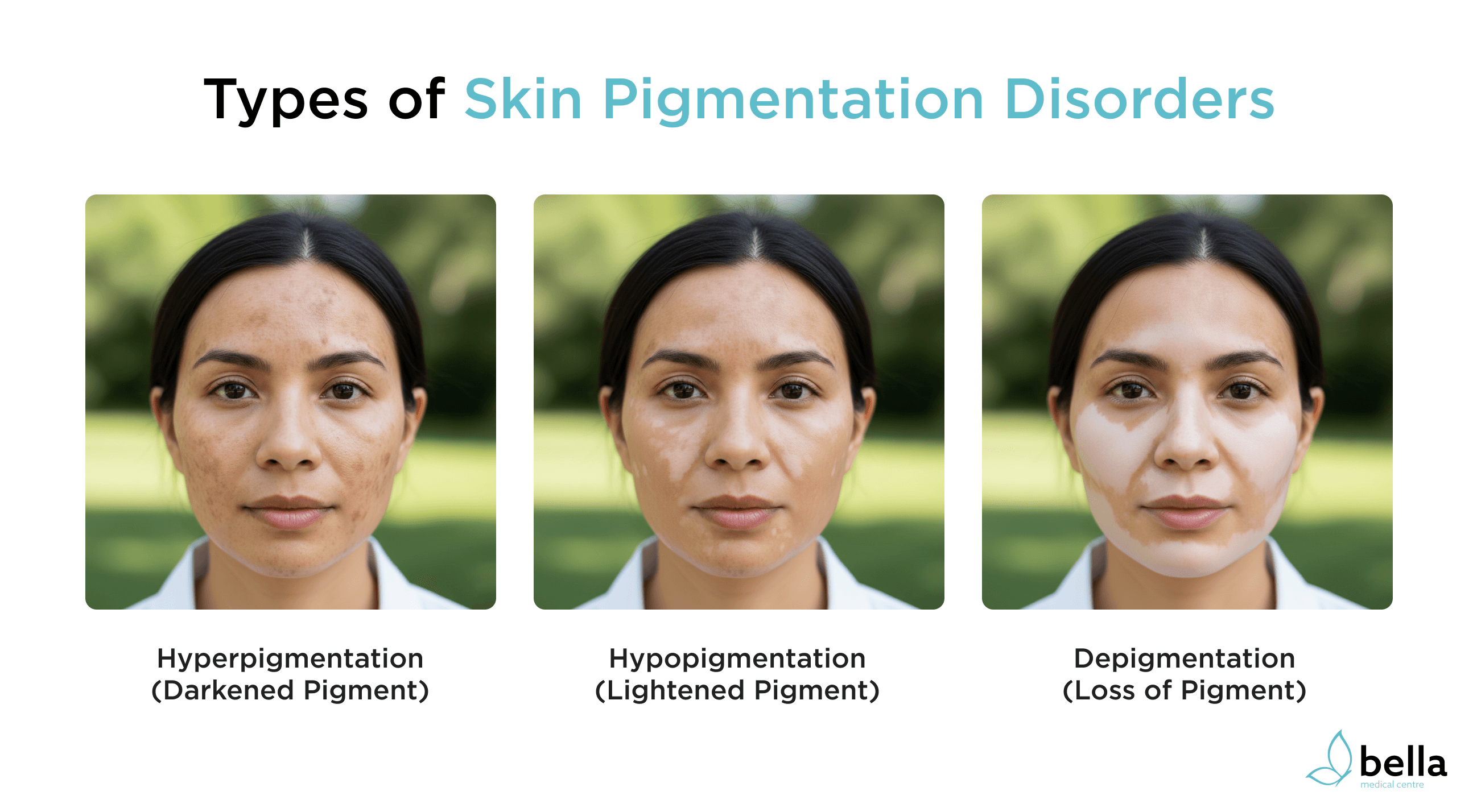
Skin pigmentation disorders occur when melanin is produced in abnormal amounts or distributed unevenly across the skin. These changes can result in either darkened, lightened, or completely colourless patches. Understanding the type of pigmentation issue can help guide the right treatment approach.
Below are the three main categories of pigmentation disorders:
Hyperpigmentation
Hyperpigmentation occurs when the skin produces excess melanin, resulting in darker patches or spots. It’s one of the most common pigmentation concerns and can appear anywhere on the body.
Common types of hyperpigmentation include:
Melasma
Often associated with hormonal changes, melasma appears as brown or grey-brown patches, typically on the cheeks, forehead, nose, or upper lip. It’s more common in women, especially during pregnancy or while taking contraceptives.
Sun spots (solar lentigines)
Also known as liver spots or age spots, these are flat, brown areas that typically appear on sun-exposed skin, such as the face, hands, shoulders, and arms. They develop gradually over time with repeated UV exposure.
Post-inflammatory hyperpigmentation (PIH)
Dark marks that remain after a skin injury or inflammation, such as acne, eczema, or a burn, have healed. This type is especially common in people with darker skin tones.
Hyperpigmentation is generally harmless but can be distressing for cosmetic reasons. It often responds well to sun protection and topical treatments.
Hypopigmentation
Hypopigmentation refers to areas where there is less melanin than normal, causing lighter patches of skin. These patches may not be completely white but appear noticeably paler than the surrounding skin.
Examples include:
Pityriasis alba
A common condition in children and teenagers that causes light, dry patches, usually on the face. It’s often linked to eczema and is not harmful.
Tinea versicolor
A fungal infection that interferes with melanin production, leading to small light or dark spots on the chest, back, or arms.
Post-inflammatory hypopigmentation
Sometimes, after skin conditions such as psoriasis or burns heal, the skin may temporarily lose pigment in the affected area.
Hypopigmentation is usually harmless and may resolve over time, but treatment depends on the underlying cause.
Depigmentation
Depigmentation is the total loss of pigment, resulting in completely white or colourless patches on the skin. Unlike hypopigmentation, there is no melanin left in the affected area.
The most recognised cause of depigmentation is:
Vitiligo
A chronic autoimmune condition where the body’s immune system attacks and destroys melanocytes. This leads to white patches that can appear anywhere on the body, including the face, hands, and genitals. The patches may spread slowly over time.
Depigmentation is usually permanent, though treatments like phototherapy, topical steroids, and cosmetic camouflage can help improve appearance and slow progression.

What are the Best Treatments for Skin Pigmentation?
The right treatment for skin pigmentation depends on the type, cause, and severity of the condition. While some forms of pigmentation may fade on their own, others require consistent care or professional intervention.
Below are the main treatment approaches, ranging from everyday skincare to advanced medical procedures.
At‑Home and Skincare Treatments
Many mild pigmentation issues can be managed with a consistent skincare routine and over-the-counter products. These treatments work best when used early and regularly.
Common ingredients found in skincare products include:
Sunscreen (SPF 30 or higher)
Daily sun protection is essential to prevent new pigmentation and prevent existing marks from darkening.
Vitamin C
An antioxidant that helps brighten the skin and reduce dark spots by slowing melanin production.
Niacinamide
Helps reduce inflammation and regulates pigment production. Often used alongside other brightening ingredients.
Retinoids (retinol or tretinoin)
Promote cell turnover to help fade pigmentation over time. Also effective for acne-related marks.
Azelaic acid
Treats both acne and pigmentation, particularly post-inflammatory marks.
Hydroquinone
A skin-lightening agent that reduces melanin production. Best used under medical supervision due to potential side effects.
Tranexamic acid
A newer ingredient that targets melasma and other forms of hyperpigmentation with fewer side effects.
Consistency is key with at-home treatments, and results can take several weeks to months to become noticeable.
In‑Clinic Medical Treatments
For deeper or more persistent pigmentation, a dermatologist or skin specialist may recommend professional treatments. These often work faster and may be combined for better results.
Popular in-clinic options include:
Chemical peels
Use acids such as glycolic or salicylic acid to remove the outer layer of skin, encouraging new, more even-toned skin to form.
Laser therapy
A laser therapy that targets melanin in the skin using focused light to break it down without damaging surrounding tissue. Often used for sun spots or stubborn melasma.
Microneedling
Uses fine needles to stimulate collagen production and improve the absorption of brightening serums. May help reduce post-inflammatory pigmentation.
Intense Pulsed Light (IPL)
A non-invasive treatment that uses broad-spectrum light to treat sun damage and uneven pigmentation.
Prescription creams
Dermatologists may prescribe stronger formulations containing ingredients like hydroquinone, tretinoin, or corticosteroids for more complex cases.
It’s important that in-clinic treatments are tailored to your skin type and pigmentation concerns. A consultation with a qualified provider is always recommended.
Preventive Skin Care and Lifestyle Tips
Preventing pigmentation is often easier than treating it. Even after successful treatment, ongoing care is important to stop pigmentation from returning.
Tips to help protect your skin:
Apply sunscreen daily, even on cloudy days. Reapply every two hours if outdoors.
Wear protective clothing, such as hats and sunglasses, when spending time in the sun.
Avoid picking at spots, scabs, or acne, as this can lead to post-inflammatory marks.
Use gentle skincare products to avoid irritation, especially if your skin is sensitive or reactive.
Stick to a consistent routine, especially when using brightening or exfoliating products.
Address underlying skin conditions (like acne or eczema) early to prevent long-term pigmentation.
Lifestyle changes such as eating a balanced diet, staying hydrated, and managing stress can also support overall skin health.




